Complications after Breast Implants Surgery – Capsular Contracture
Capsular contracture is a relatively common but often misunderstood complication associated with breast implants. It occurs when the scar tissue that naturally forms around the implant tightens and squeezes the implant, potentially causing discomfort, aesthetic changes, and the need for additional surgery.
In this blog, Sydney Specialist Plastic Surgeon Dr Bish Soliman will discuss the intricacies of capsular contracture, exploring its causes, symptoms, and the various treatment options available.
Download Dr Bish Soliman Cosmetic Breast Surgery Guide

Potential Complications after Breast Implant Surgery
While many individuals experience positive outcomes, it’s important to be aware of potential complications that can arise after the surgery. These complications can vary in severity and frequency, and understanding them is crucial for anyone considering this procedure.
- Capsular Contracture: This is one of the most common complications following breast implant surgery. It occurs when the scar tissue around the implant tightens and squeezes the implant, causing the breast to feel hard and look distorted. Treatment can range from medication to surgery to remove the scar tissue.
- Implant Rupture or Leakage: Breast implants, whether saline or silicone, can rupture or leak. A saline implant leak is usually noticeable as the saline solution is absorbed by the body, leading to a decrease in breast size. Silicone leaks can be less obvious and may require an MRI for detection. Ruptured implants typically require replacement or removal.
- Infection: Although rare, infections can occur after breast implant surgery. Symptoms may include redness, swelling, pain, and fever. Treatment often involves antibiotics, but in severe cases, the implant may need to be removed.
- Changes in Breast and Nipple Sensation: Some patients may experience increased or reduced sensitivity in their nipples or breasts after the surgery. While these changes are often temporary, they can be permanent in some cases.
- Asymmetry: Post-surgery, there may be issues with asymmetry where one breast may be a different size or shape than the other. This can be due to the natural anatomy, surgical technique, or complications like capsular contracture.
- Breastfeeding Challenges: While many women can breastfeed after having implants, some may experience difficulties. There’s also a concern about silicone implants leaking into breast milk, although research suggests this is unlikely to pose a risk to the baby.
What Is Capsular Contracture?
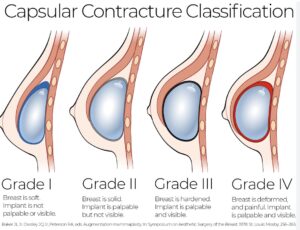
When a breast implant is placed in the body, it is normal for the body to form a lining of scar tissue around it. This lining, or capsule, is the body’s natural response to a foreign object. In most cases, this capsule remains thin and flexible. However, in capsular contracture, this scar tissue thickens, tightens and contracts around the implant, causing it to feel firm or hard, and can distort the shape and position of the implant and breast. Capsular contracture is classified into four grades, known as Baker grades.
Causes of Capsular Contracture
Understanding the causes of capsular contracture is crucial in both preventing and treating this complication effectively. Capsular contracture doesn’t arise from a single factor; rather, it’s the result of a complex interplay of various elements. Here are the contributing factors:
- Bacterial Contamination: One of the leading theories is that microscopic bacteria can adhere to the surface of the implant, forming a biofilm. This isn’t necessarily a full-blown infection but can trigger an excessive fibrotic reaction from the body. The immune system responds to this biofilm as a foreign threat, leading to an overactive scarring process around the implant.
- Haematoma/Seroma: The presence of blood (haematoma) or fluid (seroma) around the implant, especially soon after surgery, can significantly increase the risk of capsular contracture. This accumulation can irritate the tissues and stimulate a more aggressive fibrotic response.
- Implant Placement and Type: The risk of capsular contracture can also be influenced by the specifics of the implant itself. This includes whether the implant is placed subglandular (above the muscle) or submuscular (below the muscle), and the characteristics of the implant – whether it’s smooth or textured, silicone or saline. Textured implants, for instance, have been shown in some studies to have a lower risk of capsular contracture compared to smooth implants, possibly due to their surface texture disrupting the formation of tight scar tissue.
- Genetic Factors: Genetics may also play a role. Some individuals are naturally predisposed to forming more aggressive or thicker scar tissue, which can contribute to the development of capsular contracture.
- Surgical Technique: The methods and precision used during the implant surgery are critical. Factors like how the implant pocket is created, how the implants are handled, and ensuring a sterile environment can all impact the likelihood of capsular contracture developing.
- Post-Surgical Complications: Any complications following the surgery, such as infections, can elevate the risk. An infection can exacerbate the body’s inflammatory response, leading to more pronounced scar tissue formation.
- Immune System Response: Finally, an individual’s unique immune system response to the foreign material (the implant) can vary significantly. Some immune systems may react more strongly than others, leading to a more robust fibrotic reaction.
Treatment and Management
Treating capsular contracture effectively requires a tailored approach, depending on the severity and individual circumstances of each case. The Baker grading system is commonly used to classify the severity of capsular contracture, ranging from Grade I (breast is soft and appears natural) to Grade IV (breast is hard, painful, and appears abnormal). Here’s a closer look at the treatment options based on the severity of the condition:
- Medication: In the early stages or for milder cases (Baker Grade I and II), certain medications can be beneficial. Leukotriene inhibitors are sometimes prescribed. These medications are traditionally used for conditions like asthma but can help in reducing inflammation and may slow down the progression of capsular contracture.
- Capsulectomy: For more severe cases (Grade III and IV), surgical intervention is often necessary. A capsulectomy involves the surgical removal of the entire scar tissue capsule surrounding the implant. This procedure can alleviate pain and distortion caused by the contracture. Depending on the situation, Dr Bish Soliman may also perform a capsulotomy, which is the surgical release or scoring of the capsule, though this is less common.
- Implant Replacement or Removal: In conjunction with capsulectomy, or as a standalone treatment, replacing or removing the breast implant might be necessary. Implant replacement can involve switching to a different type or texture of implant, which might be less likely to cause a recurrence of capsular contracture. In some cases, patients may opt for implant removal, either due to personal preference or if the risk of recurrent contracture is high.
- Massage and Physical Therapy: For less severe contracture, or as a preventive measure post-surgery, breast massage and physical therapy may be recommended. These techniques aim to keep the capsule flexible and prevent it from tightening around the implant. However, it’s important to note that this approach is more effective in the early stages of capsular contracture and is less likely to be beneficial for advanced cases.
- Ultrasound Therapy: Some recent studies suggest that ultrasound therapy might be effective in treating capsular contracture by reducing inflammation and promoting healing. However, this is a relatively new area of treatment and should be considered experimental.
- Preventive Measures: In addition to these treatments, Dr Bish will employ various preventive measures during the initial implant surgery to minimise the risk of capsular contracture. This includes using specific surgical techniques, selecting the appropriate type and placement of implants, and ensuring a sterile surgical environment.
Capsular Contracture Prevention
While it’s not always possible to prevent capsular contracture, certain measures can reduce the risk:
- Antibiotic Prophylaxis: Using antibiotics during and after surgery to reduce the risk of bacterial contamination.
- Surgical Technique: Employing meticulous surgical techniques to minimise tissue trauma and contamination.
- Implant Selection: Choosing the appropriate implant type and placement for the individual.
- Post-Operative Care: Following Dr Bish’s instructions for post-operative care, including any recommended exercises or massages.
It’s important for patients to have a thorough discussion with Dr Bish Soliman about the risks of capsular contracture and the steps that will be taken to minimise these risks before undergoing breast implant surgery. Regular follow-up appointments are also crucial for monitoring the condition of the implants and the surrounding tissue.
The Role of Surgeons in Managing Capsular Contracture
Surgeons play a critical role in the management of capsular contracture. They have the expertise to diagnose and treat this condition effectively. Additionally, they can provide guidance on preventive measures and educate patients about the signs and symptoms to watch out for. Regular follow-up appointments with Dr Soliman are essential to ensure the long-term success and satisfaction of your breast implant treatment.
By working closely with Dr Soliman and following his recommendations, you can minimise the risk of complications and achieve the desired outcome for your breast augmentation journey.
FAQs about Capsular Contracture
How common is capsular contracture after breast implant surgery?
- The incidence of capsular contracture varies, but it’s one of the more common complications of breast implant surgery. The rates can differ based on various factors, including surgical technique, type of implant, and individual patient characteristics. It’s estimated to occur in about 10% of cases, but this can vary.
Can capsular contracture occur years after surgery?
- Yes, capsular contracture can develop at any time after the surgery. While it often occurs within the first few months to years, it can also develop several years post-surgery. Regular follow-up and self-examination are important for early detection.
Are there any specific symptoms to watch for indicating capsular contracture?
- The primary symptoms include firmness or hardening of the breast, pain or discomfort, and noticeable distortion or asymmetry of the breast shape. In advanced cases, the implant may feel tight or be visibly misshapen.
Is capsular contracture more common with silicone or saline implants?
- Historically, the risk of capsular contracture was thought to be higher with silicone implants compared to saline implants. However, with advancements in implant technology, the difference in risk between the two types has become less clear. The choice of implant should be discussed with Dr Bish Soliman.
Can capsular contracture resolve on its own without treatment?
- Capsular contracture typically does not resolve on its own and may progressively worsen if left untreated. Early stages might be managed with non-surgical approaches, but more severe cases usually require surgical intervention.
Further Reading about Breast Implants Surgery with Dr Bish Soliman
- Read more about Bra Cup Sizes related to Breast Implant Sizes
- Read more about How to Choose the Best Bra after Breast Augmentation
- Read more about Round vs Anatomical Breast Implants
- Read more about Why Dr Bish Uses Motiva Breast Implants
- Read more about Sports Bra After Breast Augmentation?
- Read more about Silicone Breast Implants
Medical References about Capsular Contracture
- What is capsular contracture and how can it be treated?
- Capsular Contracture after Breast Augmentation
- Capsulectomy: Surgery to Soften Breast Implants
- Capsular contracture in the modern era
- Prophylactic Leukotriene Inhibitor Therapy for the Reduction of Capsular Contracture in Primary Silicone Breast Augmentation